Can Cataract Symptoms Affect Your Mental Health?
One of the most common challenges faced by older people is blurry eyesight and the development of cataracts. Cataracts, while considered a normal part of the ageing process, are also one of the culprits for vision loss in seniors.
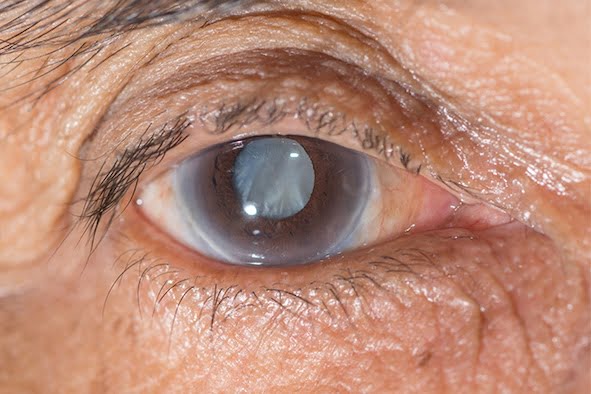
So what happens when we age? The eye’s natural lens becomes cloudy and hard over time, evolving from being flexible and crystal clear. This dilutes clear vision and everything becomes blurry and dull. Because of this poor eyesight, a person affected with cataracts will find it difficult to do usual day-to-day activities without corrective lenses.
For people with cataracts, seeing through cloudy lenses is more like looking through a frosty or fogged-up window. The clouded vision caused by cataracts makes it more difficult to read, engage and interact with friends, or drive a car, especially in low-light situations.
As most cataracts develop slowly, they rarely disturb your vision in the early stages. At first, the cloudiness in your vision might not be really noticeable as it only covers a tiny speck of the eye’s lens. But over time, your vision impairment will worsen, as more of your lens gets clouded, distorting the light passing through the lens. This may lead to more noticeable symptoms.
According to MayoClinic, the common cataract symptoms include:
- – Vision that’s clouded, blurred or dim
- – Increasing difficulty with vision at night
- – Sensitivity to light and glare
- – Need for brighter light for reading and other activities
- – Seeing “halos” around lights
- – Frequent changes in eyeglass or contact lens prescription
- – Fading or yellowing of colours
- – Double vision in a single eye
Types of cataracts
Cataracts affecting the centre of the lens (nuclear cataracts)
This cataract may at first cause more nearsightedness or even lead to a temporary improvement in your reading vision. However, with time the lens progressively yellows and becomes more dense, further clouding vision.
With slow progression, the lens may even turn brown. At an advanced stage, this yellowing or browning of the lens can lead to difficulty distinguishing between shades of colour.
Cataracts that affect the edges of the lens (cortical cataracts)
A cortical cataract starts as whitish, wedge-shaped opacities or streaks on the outer edge of the lens cortex. With slow progression, they extend to the centre, interfering with the light going through the centre of the lens.
Cataracts that affect the back of the lens (posterior subcapsular cataracts)
It starts as a small, opaque area, usually forming near the rear of the lens, and is normally right in the path of light. A posterior subcapsular cataract often disrupts your reading vision, decreases your vision in bright light, and causes halos around lights at night. These types of cataracts often progress faster than other types.
Cataracts you’re born with (congenital cataracts)
On the other hand, some people are born with cataracts or they develop them during childhood. These may be genetic or associated with an intrauterine infection or injury. These cataracts may also be caused by certain conditions such as; myotonic dystrophy, galactosemia, neurofibromatosis type 2 or rubella. Generally, congenital cataracts do not always affect vision. If they do, they’re usually removed as soon as they are detected.
What causes cataracts?
The lens of your eye is mostly water and proteins. Over time the proteins break down and hang around in your eye. These lingering proteins are what makes your lens cloudy and makes it hard to see clearly. Though a typical part of ageing — it is unpleasant.
That said, here are some examples of things that can speed up the formation of cataracts:
- – Diabetes
- – Steroids, in common prescriptions to treat conditions like arthritis and lupus
- – Phenothiazine drugs, used to treat a variety of conditions for example chlorpromazine (Thorazine®) for treating schizophrenia and bipolar disorder
- – Eye injuries or surgeries
- – Radiation treatment targeting the upper body; and
- – Spending a lot of time in the sun without eye protection, like sunglasses.
Cataracts are the main cause of visual impairment in the world, accounting for 51% of blindness and 33% of visual disability. Over visual impairment, cataracts are also related to difficulties in activities of daily living, social engagement, independent mobility and increased risk of falls and injury.
Cataracts and their impact on mental health
Evidence has shown that cataracts are further associated with multiple psychological comorbidities, including elevated rates of anxiety and depression. Previous studies have also suggested the correlation between depression and visual impairment indicating a longitudinal association between visual impairment and depressive symptoms.
To be more specific, a study by Ophthalmologists at the University of Washington has suggested that cataract extraction is associated with a lower risk of developing dementia among older adults. The study assessed 3,038 adults who were 65 years of age or older with cataracts and enrolled in the Adult Changes in Thought study.
Since depression is also common in the elderly, it looked at older adults. The link was independent of other factors discovering that older adults were the worst affected.
The study helped shed further light on the complex relationship between aging, vision loss, cataract, and depression and suggested that there may be a role for cataract surgery in improving mental health in the elderly. There is also established evidence of an association between cataracts and depression in this demographic.
As indicated by the Global Burden of Disease Study, depressive disorders are the third non-fatal leading contributors to the global disease burden. Depression is also associated with functional impairment, risk of dementia, and increased mortality.
In clinical practice, depressive symptoms are common among patients with eye disease. However, depression is often left unrecognised or untreated in the ophthalmological clinic, which can adversely influence treatment and therapy outcomes further hampering the quality of life.
It may seem unusual but our eyes are an extension of the brain. Hence maintaining good eye health may have an added effect in keeping the brain healthy, too. That maintenance might include the treatment of cataracts, when the lens of our eyes cloud up, obscuring and darkening our vision.
Studies have shown that nearly 30% of people over 65 who had their cataracts surgically removed were less likely to develop dementia than those who didn’t. Inherently, this lowered risk was seen even after other risk factors for dementia were controlled for, with the effect seeming to last at least a decade later.
In the study “Association Between Cataract Extraction and Development of Dementia” published in JAMA Intern Med. on December 6, 2021, analysts have theorised that the decrease in risk might happen because people’s improved vision post-treatment helps keep the brain active. On the other hand, it could also be the result of the treatment specifically by improving people’s ability to process blue light, which could reawaken cells in the retina associated with healthy sleep and cognition.
As further proof for that theory, it’s suspected that individuals suffering from other eye disorders involving the retina are at higher risk for dementia as well.
Now, how do we treat cataracts?
There is no better or more effective way of eliminating cataract than undergoing surgery. In fact, it is the best treatment available, being the most common operation conducted in the world today, averaging at 15 million procedures every year.
Fortunately, cataract surgery is generally an effective, safe, low-cost and effective intervention for treating such visual impairment. The potential benefits of cataract surgery towards alleviating the related burden of psychological symptoms have been documented.
The procedure of removing cataracts involves implanting a clear artificial lens to replace the affected natural lens. The process is fast, usually lasting in less than an hour, depending of course, on the severity of the condition. There has been marked evolution in lens technology and if suitable, freedom from both distance and reading glasses, permanently, is now possible.
If you want to regain your vision and freedom of movement, you can take advantage of Freedom Eye Laser’s cutting-edge surgical technology. Headed by our Founder and Medical Director Dr James Genge, you can say goodbye to your glasses and poor eyesight, especially with his expertise and the premium, latest generation intraocular lenses he uses.
Contact us to hear more about your options today.



